Cardiovascular Diseases
Cardiovascular diseases (CVD) refer to conditions affecting the heart and blood vessels including coronary artery disease (CAD) and heart failure (HF). Despite considerable diagnostic and therapeutic advances in CVD, they remain the leading cause of morbidity and mortality globally.
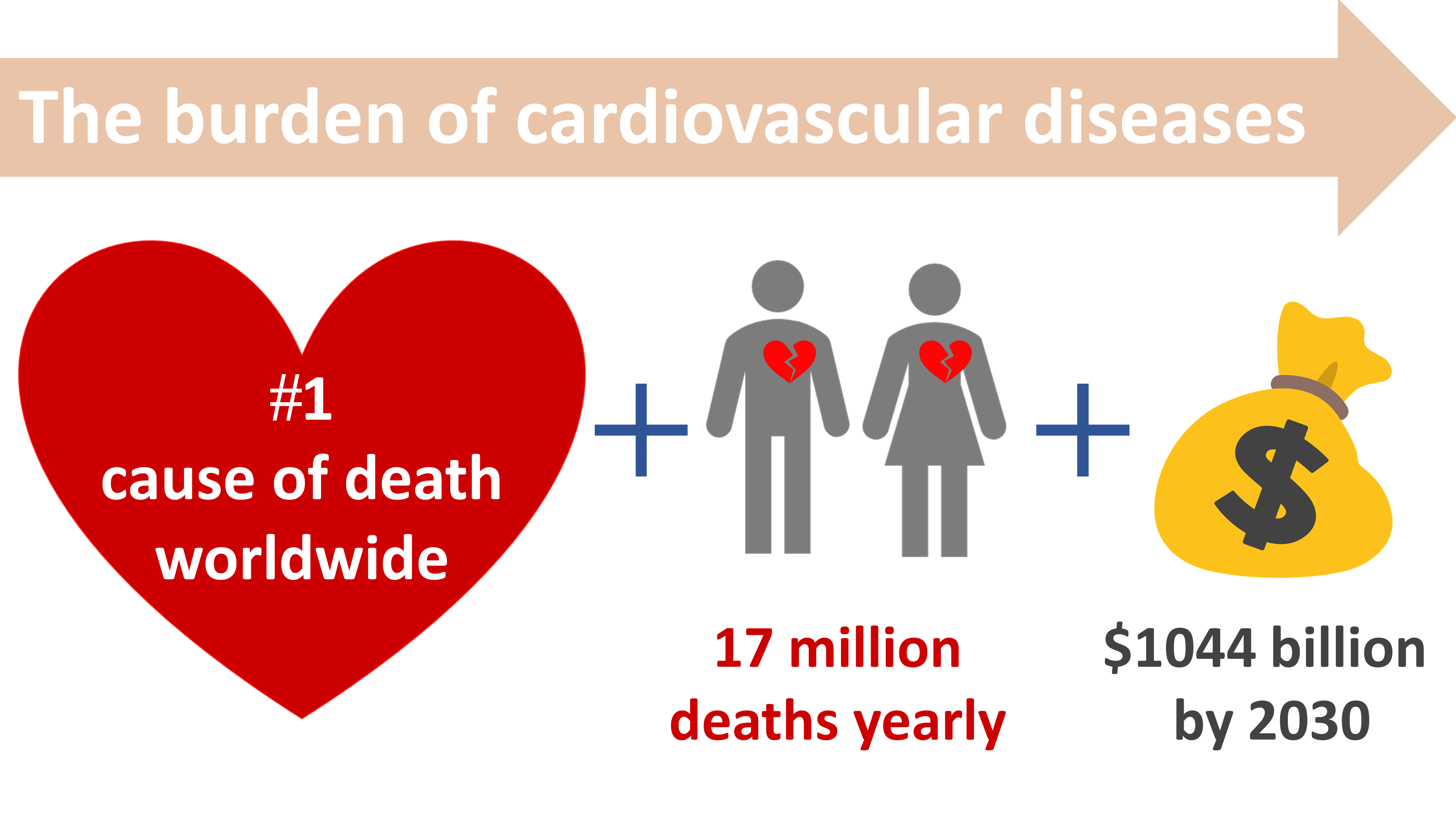
CVD remain the leading cause of mortality despite advances in the management.
According to the World Health Organisation (WHO), CVD claim 17.7 million of lives yearly, altogether accounting for 31% of all global deaths. Usually considered to mostly affect the elderly population (≥ 65 years), the prevalence of CVD in young individuals (18-50 years) is rising1. This is due to the increase prevalence of risk factors among young adults living in the Western world. These risk factors include high blood pressure, diabetes mellitus, smoking, obesity and physical inactivity. The financial projections of the global cost for CVD were estimated at $1044 billion by 20302. Considering the burden of CVD, innovative methods to improve the management of CVD are urgently needed.
Mosaiques Diagnostics is dedicated to improving patients' quality of life by developing novel technologies for the diagnosis and therapy of coronary artery disease and heart failure using a personalised medicine approach.
Mosaiques Diagnostics is dedicated to developing novel technologies to improve the diagnosis and therapy of Coronary Artery Disease and Heart Failure.
Coronary Artery Disease
Coronary artery disease (CAD) is characterised by plaque formation or atherosclerosis in the arteries. It is a major public health concern in developed countries. Although a significant improvement in the management of CAD was observed, the prevalence of CAD is still on the rise due to demographic transition and increased survival rates. The aetiological diversity of CAD makes it challenging to fully decipher complex pathological processes based on single biomarkers.
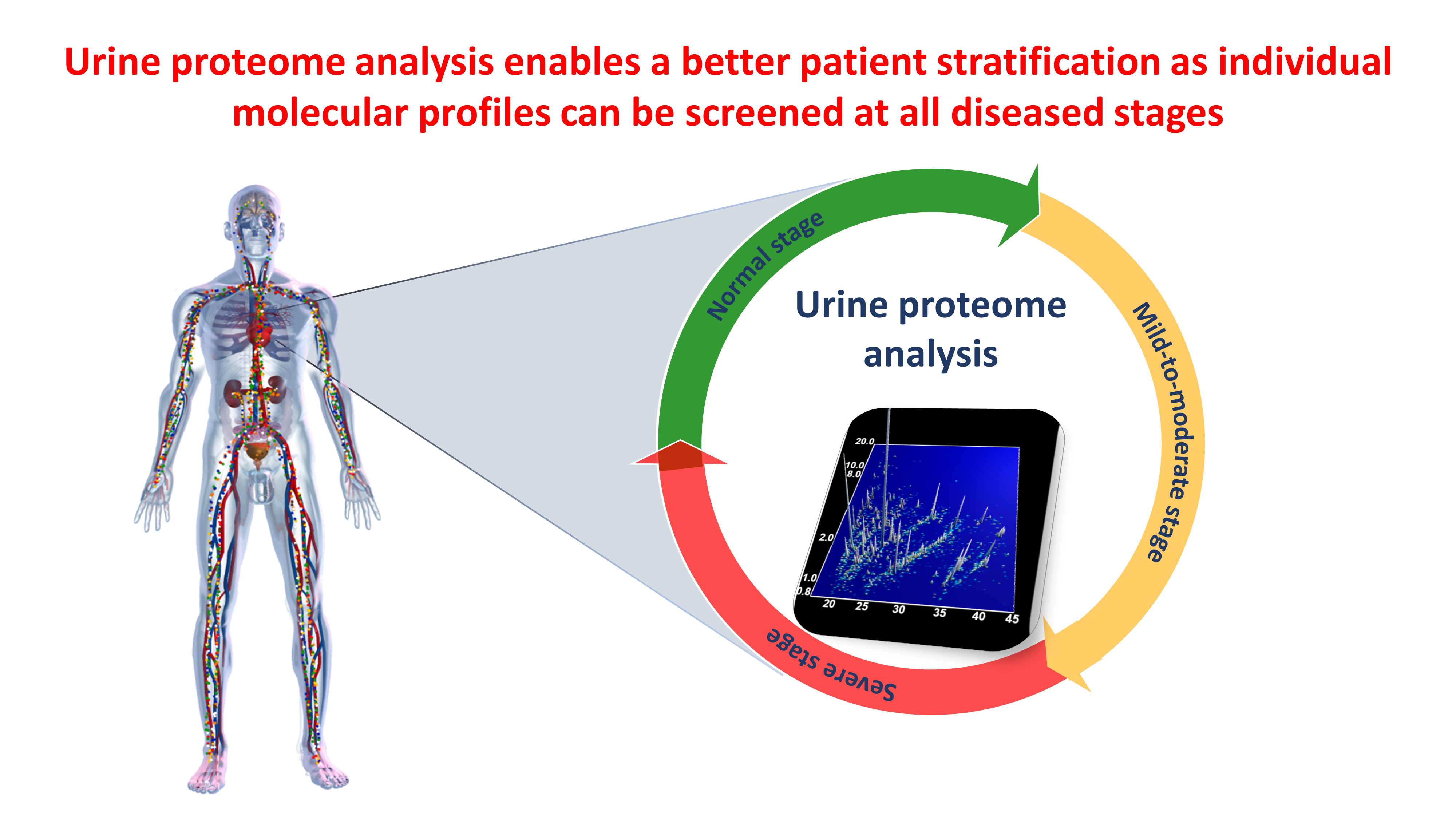
The diagnosis of CAD is challenging. Current non-invasive diagnostic modalities are of moderate value. Reliable biomarkers for the diagnosis and prediction of CAD could lead to improved risk stratification, enable earlier interventions and enable the monitoring of treatment efficacy. We have identified clinically relevant biomarker signatures using urine proteome analysis that improve the diagnosis and prediction of CAD or its associated complications3-7.
Heart Failure
Heart failure (HF) is a major and escalating public health concern worldwide affecting over 37 million individuals globally8. It is associated with unprecedented economic costs globally. Heart failure is a multi-factorial condition characterised by the heart’s inability to pump sufficient amount of blood to meet the requirements of the body. Although significant advances in the treatment of HF have clearly improved patient survival, its prevalence is still on the rise.
In ageing populations, early stratification of subjects with HF with unprecedented accuracy, when prevention is still possible, is of paramount importance. The early classification of patients will enable timely personalised pharmacological interventions accompanied by non-pharmacological interventions to reduce risk factors e.g. by life style changes (exercise, healthy diet). This may prevent or at least delay progression and thus reduce mortality and morbidity, promote healthier ageing and a more active life.
Our unique urine proteome analysis has enabled us to break beyond the status quo and provide an early stratification of individuals with HF9-18.
REFERENCES:
- Anderson and Vasan. Nat Rev Cardiol. 2018; 15(4):230-240.
- Mozaffarian et al. Circulation. 2015; 131:e29-322.
- Delles C et al. J Hypertens. 2010; 28: 2316-2322.
- Brown et al. Proteomics Clin Appl. 2015; 9: 610-617.
- Silva et al. Am J Clin Nutr. 2015; 101(1):44-54.
- Neisius et al. BMC Cardiovasc Disord. 2016; 16:70.
- Htun et al. PLoS One. 2017; 12:e0172036.
- Ziaeian B et al. Nat Rev Cardiol. 2016; 13:368-378.
- Kuznetsova T et al. Eur. Heart. J. 2013 ; 33 :2342-2350
- Zhang ZY et al. Int J Cardiol. 2014; 176: 158-65.
- Farmakis D et al. Eur. J. Heart. Fail. 2016; 18:822-829.
- Zhang ZY et al. PLoS One. 2016; 11(12):e0167582
- Rossing K et al. PLoS One. 2016; 11(6):e0157167
- Zhang ZY et al. J Am Heart Assoc. 2017; 6: pii:e005432
- Ferreira JP et al. Circ Heart Fail. 2019;12(5):e005897.
- Campbell RT et al. ESC Heart Fail. 2020;7(4):1595-1604.
- He T et al. Clin Transl Med. 2021;11(1):e267.
- He T et al. Eur J Heart Fail. 2021;23(11):1875-1887.



